‘The best strategy is to focus on the healthy and uninfected population and keep them uninfected’– Dr Sanjeeb Sapkota
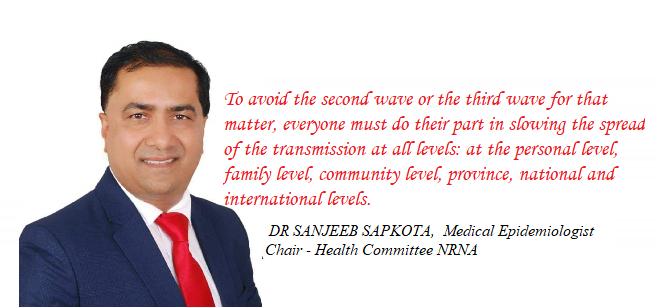
DR SANJEEB SAPKOTA is a Medical Epidemiologist and has been working in the public health sector for the past 20 years. After graduating from the Tribhuwan University as a medical doctor, he worked in World Health Organization (WHO) for several years, and later with a number of other public health agencies. He has served as a consultant to Ministries of Health of several countries in Europe, Africa and Asia. He has published several books including on pandemic. Currently he leads the Health Committee of Non-Resident Nepali Association (NRNA). He lives with his wife and two sons in Atlanta in the United States. He spoke with BHAGIRATH YOGI and JAGAN KARKI on contemporary issues. Excerpts of the interview:
You have been monitoring the impact of the pandemic in the Nepali community around the world on the Nepali diaspora. What is the latest situation?
There are an estimated over 8 million people of Nepali origin spread across different countries around the globe. Close to 2 million of them are in different countries of Arab nations of the Middle East of Saudi Arabia, Qatar, Kuwait, UAE, Bahrain, Oman, and Malaysia. Close to 3 million are in India and other South Asian countries. America, Canada, UK, Australia, New Zealand –the English speaking countries– have around 1.5 million people, and the rest in Africa, East Asia, and Europe. All of them are impacted by the Corona pandemic in varying ways.
As of Aug 30, there were an estimated over 71 thousand Nepalis infected worldwide including in Nepal. An estimated 53 thousand of them have recovered, bringing the recovery percentage this week at 75. We lost 194 Nepali outside of Nepal so far, and 215 in Nepal with a total of 410.
Most of them had underlying medical conditions and were elderly people. But some have died in their 20s and 30s. The United Kingdom, United States, United Arab Emirates and India are the countries where the majority of these deaths have occurred. Deaths also occurred in Qatar, Kuwait, Saudi Arabia, South Africa, Turkey, Denmark and The Netherlands. The ex-Gurkha Nepali population has been disproportionately affected by the pandemic. Most Nepalis by now know how the infection is transmitted and what needs to be done to prevent it. Wearing a mask when out in the public, washing hands thoroughly before touching the nose and mouth, and maintaining social distancing is what is needed to prevent the spread of the Covid-19.
The NRNA is said to be slow to respond to the Covid-19 crisis as it affected the Nepali diaspora. Now, how you are supporting the community in more than 80 countries around the world?
The magnitude of the pandemic and the speed at which it accelerated was unmatched by any level of interventions. No government, agency or organisation could fight this alone, let alone the NRNA. Akin to uncontrollable wildfire where any number of fire fighting trucks and the aeroplane would not extinguish the fire, this pandemic would not be slowed by any amount of interventions. That said we could not afford to be complacent. From January 2020 when the infection rate surged in China, NRNA and its health committee rolled out an awareness campaign on how the virus is transmitted and what could be done to prevent the chain of transmission. We organized hundreds of live broadcasts via social media on what people need to do to prevent the infection. We send out advisory via audio, video, digital, and other media. We procured thousands of testing kits and personal protective equipment and handed those to the Nepal government. We established the health team in the Middle East, Africa, Europe, India, the United States, and provided telehealth and consultations to Nepali community. But no matter how much we do, it is not enough. But the key is to not stop the combat no matter how invincible the menacing virus appears. That day is not far when this ‘fire of viral transmission’ would die out.
You live in the US and have watched the response to the pandemic closely. Where do you think the US missed in dealing with the Covid-19? What are the lessons learnt?
The United States and most other countries missed many opportunities to contain the virus. But the major miss was the underestimation of the virulence and the infectiousness of the virus. Hardly any country or organization prepared for this enormous size of the beast. Not that the United States did not prepare for the pandemic. Fifteen years ago in 2005, it prepared heavily against the potential influenza virus called bird flu or H5N1 strain of influenza. The country assumed this virus is going to cause the pandemic and made significant preparations at all levels. The outbreak never crossed the animal realms and did not cause sustained human transmission.
Five years later in 2010, the first pandemic of the 21st century happened but the virulence of the virus causing it, the H1N1 strain of influenza, was mild. It was infectious but not as deadly as the current Coronavirus is. People blamed the government for overreacting. Since 2010, several strains of viruses posed threat to be pandemics, such as H7N9 influenza, Middle East Respiratory Syndrome (MERS), and others, but those did not cause a pandemic. When the Coronavirus outbreak occurred in Wuhan, China, many assumed it is going to just cross its border to the neighboring countries, and just be some pockets of outbreaks. The health officials assumed it is not going to be a pandemic and might not be as virulent as it is now. Many lessons are drawn out of this gigantic crisis. First, no one country could fight this alone and every country needs to unite.
Within any country, all levels of government — ward/local, village, municipality, district, county, regional/province and national —all need to effectively unite and communicate freely and frequently, need to collaborate with every organisation, small or big, should bring on board the professional, semi-professional and non-professional groups, media, schools, students, scouts and all. I mean all. This is a crisis of humanity and each human being within a country and among the country has a role to play in slowing the spread and eventually stopping it.
Ethnic minorities are said to have been affected by the Covid-19 disproportionately in countries like the US and UK. Why is it so?
Blacks, Hispanics, and Asian minorities in the UK and the USA are disproportionately impacted in several other health conditions such as heart disease, diabetes, and the current infectious disease caused by Coronavirus. Inadequate access to health, delay in seeking medical attention, lower socio-economic status contribute to higher infliction among the minorities from various health issues. Lack of knowledge, or having inadequate of it, on how the virus is spread and not taking effective measures needed to prevent them are the major driver of the pandemic. The same is true for other chronic and infectious diseases.
The language barrier, lack of minority’s representation in the planning and execution of pandemic mitigation, lack of educational materials targeted for minorities, higher amount of pre-existing medical conditions among the minorities, the inadequacy of the social leaders within the minorities to connect to the majority and the lack of the government to recognize the plight of the minorities — all compound together to the disproportionate impact on them. Low income, low education are often common among ethnic minorities. These are common social determinants of health, whether for heart disease or coronavirus infection.
How do you think the diaspora communities can help their country of birth especially in South Asia. Could you give us an example?
An estimated over 5000 Nepali medical doctors and tens of thousands of Nepali nurses provide services in various countries globally. Thousand other allied health workers practice around the world. They have expertise including in the prevention, treatment, and promotion of health. They could provide technical guidance to government agencies, professional organizations and the public; they could provide telehealth consultations; they could organise health camps in different rural parts of Nepal.
They could identify areas where the infection rate is increasing and raise funds to fund prevention campaign, telehealth consultations and mental health experts could provide counseling and guidance. Less the people are infected, easier it is to manage the pandemic, less the hospital beds occupied, less the risk of the infection to the public, doctors and nurses.
The best strategy is to focus on the healthy and uninfected population and keep them uninfected. This will tremendously lower the burden on limited finite medical care and medical care providers. This entails a resilient laboratory system where testing is rapid and in large throughput. The simultaneous focus should be the rapid treatment of those who are infected and the management of the mental health of both the infected and their family and relatives.
The 2nd Global Nepali Health Conference we are organizing during Sept 18-20, 2020 is expected to bring a large number of people and organisations who have stakes in the health of Nepali people. This will be another milestone in strengthening the coalition of global Nepali health professionals for our motherland.
South Asian communities enjoy get-together and partying as big festivals like Dashain and Diwali are around the corner. What would be your advice for them to protect themselves?
Any gathering of unknown people in enclosed spaces within a room or hall needs to be avoided. The risk of the spread of the infection is multiple folds in a confined space than outdoor. This does not mean we need to cancel the cultural festivities. Dashain and Diwali could still be celebrated among family members living in the same household. Until the vaccine is out there, and until we have people vaccinated, the large gathering needs to be avoided.
People are now talking about the ‘second wave’ of the Covid-19? How serious it will be and how can we cope in such a situation?
The second wave is the increase in the number of infected people among those who were largely uninfected and healthy before. Once the curve of the rate-of-infection flattens and bends downwards people tend to believe the chain of transmission has slowed or stopped. They then tend to come out in the public. This put the previously healthy people at high risk to be infected. This increases the curve again, and this is what constitutes the second wave.
People tend to believe the second wave is due to the virus getting mutated or getting deadlier, but it is the same virus. The severity of the virus is the same as before, it is just more people are now infected. Now, the virus could mutate and become more virulent than it is now, but the current second waves we are seeing are caused by the same virus. To avoid the second wave or the third wave for that matter, everyone must do their part in slowing the spread of the transmission at all levels: at the personal level, family level, community level, province, national and international levels.
Effectively covering face and nose while in public places, not touching face before washing hands with soap and water, remaining a safe 2-meters away from any stranger are different measures done at the personal level to avoid getting infected or spreading the infection to others. Also if a person is showing symptoms or suspects he or she is exposed to the infection, then they need to seek immediate medical attention and remain in the home confinement for 14 days.











Facebook Comments