New Framework Redefines Obesity Diagnosis by Prioritizing Waist-to-Height Ratio Over BMI
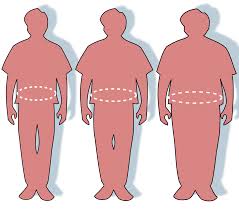
July 14, 2024 — Researchers have introduced a groundbreaking framework for diagnosing and managing obesity, emphasizing the distribution of body fat rather than relying solely on Body Mass Index (BMI). Published in the journal Nature Medicine, this new approach focuses on fat accumulated in the abdomen, measured by the waist-to-height ratio, which they assert is a more accurate predictor of cardiometabolic health risks.
The European Association for the Study of Obesity (EASO) has endorsed the framework, which introduces a waist-to-height ratio higher than 0.5 as a key criterion for diagnosing obesity, alongside a BMI range of 25-30. This shift marks a significant departure from traditional methods that primarily use BMI, with a cut-off value of 30 for obesity.
“The choice of introducing waist-to-height ratio, instead of waist circumference, in the diagnostic process is due to its superiority as a cardiometabolic disease risk marker,” the researchers stated. They highlighted that abdominal fat accumulation is a more reliable predictor of health deterioration compared to BMI, even for individuals who do not meet the current BMI threshold for obesity.
The framework challenges the existing guidelines, which are based on studies including participants who meet specific BMI cut-off values rather than a comprehensive clinical evaluation. “The basis for this change is the recognition that BMI alone is insufficient as a diagnostic criterion, and that body fat distribution has a substantial effect on health,” the authors wrote.
The new approach aims to address the risk of undertreatment among patients with a low BMI but high abdominal fat. By incorporating waist-to-height ratio into the diagnostic process, the researchers believe that healthcare providers can better identify and manage individuals at risk of cardiometabolic complications.
Implementing this new framework could lead to more precise and effective obesity management, ultimately improving health outcomes for patients who might otherwise be overlooked under the current BMI-based system. The EASO and the study’s authors advocate for its adoption, emphasizing the need for a more nuanced understanding of obesity and its health implications.











Facebook Comments