Difference between virus variants and strains
Some virus experts might not consider viruses to be alive. Yet viruses can reproduce, according to sciencenewsforstudents.org.
To do so, they hijack the cells of a host. They borrow the “machinery” in the host’s cells to copy the virus’ genetic code.
Those host cells may spit out hundreds or thousands — even millions — of copies of the original virus.
These new viruses then go on to infect more cells. Maybe the host will also sneeze out the viruses or otherwise release some to infect other potential hosts.
And those hosts might be anything from people or plants to bacteria.
But each time a virus is copied, there’s some risk the host’s cell will make one or more errors in the genetic code of that virus, according to sciencenewsforstudents.org.
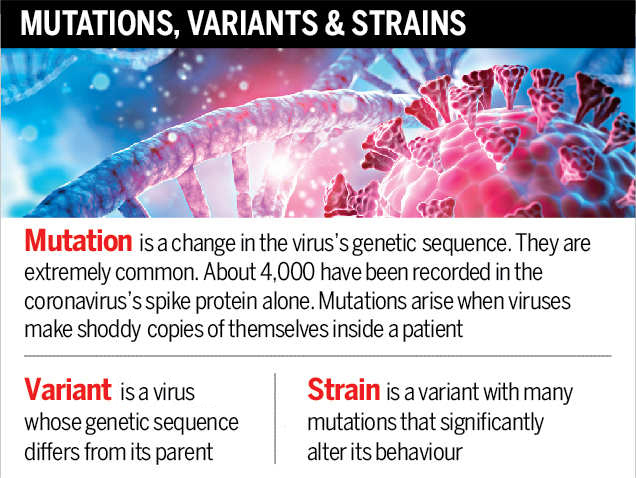
These are known as mutations. Each new one alters the genetic blueprint of the virus a bit. Mutant viruses are known as variants of the original.
Many mutations won’t affect how a virus works. Some might be bad for the virus. Others might improve how well the virus can infect a cell, or help the virus evade its host’s immune system. A mutation might even allow the virus to resist the effects of some therapy. Scientists refer to such new-and-improved variants as strains.
Keep in mind that all strains of a virus are variants. Not all variants, however, are different enough to qualify as a new strain.
And although coronavirus variants made news throughout much of the COVID-19 pandemic, any virus runs the risk of spawning new variants through mutation.
Indeed, mutations are one basis of evolution. Mutations that don’t benefit an organism (or virus), often die out. But those that make an organism more fit — better adapted to its environment — tend to become more dominant.
Coronavirus variants
Anthony Fauci heads the National Institute of Allergy and Infectious Diseases. It’s in Bethesda, Md. Every time a virus infects someone, viral copying — also known as replication — goes on.
And as each new copy is made, he notes, there’s the risk of a new variant developing. He spoke August 12 on National Public Radio’s Morning Edition to discuss concerns about the coronavirus.
“A virus will not mutate if you don’t allow it to replicate,” he explained. “And when you have people getting infected and spreading it through the community, the virus has ample opportunity to do that.” Let enough people get infected, and “sooner or later,” he said, a more dangerous form of the virus may evolve. That’s why virus experts have been pushing vaccines, use of masks and social distancing. These cut the risk of new infections, which will limit the risk of new copying errors.
Scientists refer to some new versions of the coronavirus as “variants of concern.” Compared to the original virus, these variants might infect or spread between people more easily, respond less well to treatments or impair how well vaccines work against the virus.
A more serious class of viruses are so-called “variants of high consequence.” Treatments or precautions work far less well against these viruses than they had against earlier forms of the virus. For instance, the new variants might resist current vaccines. They may not show up well in current tests. They might even cause more severe disease.
As of August 2021, no coronavirus variants of high consequence have emerged anywhere in the world. But there were four variants of concern. As one after another evolved, scientists began referring to them with letters of the Greek alphabet: alpha, beta, gamma and delta.
That last one has been especially troubling. According to the U.S. Centers for Disease Control and Prevention, or CDC, the delta variant spreads much faster than other variants. It seems to cause more severe disease. It also responds less well to treatment with lab-grown antibodies. The good news: COVID-19 vaccines appear to work well at limiting severe disease or death from this variant.
Other viral variants and strains
The influenza virus mutates rapidly. The new strains spawned by those changes are one reason people need flu shots every year. The latest flu vaccines have been developed to target new variants.
Variants usually develop within a host because viruses are error-prone. This is especially true for RNA viruses, such as coronaviruses and flu viruses.
And some variants may prove better suited to reach particular target tissues. That’s what Holly Hughes and her team found. Hughes works for the CDC in Fort Collins, Colo. There she focuses on decrypting the genetic code of viruses.
She was part of a team that did this for EEEV. That’s short for the eastern equine encephalitis (En-seff-uh-LY-tis) virus. Hughes notes that it is “one of the deadliest mosquito-borne diseases in the United States.”
Few people become infected by this virus. But about a third of those individuals die. And those who survive can be left with long-term physical or mental problems.
Hughes’ team sampled the virus from a woman who got EEEV during a 2019 epidemic — and didn’t survive. The researchers turned up a number of EEEV variants in her blood. The team also sampled fluid from around her brain and spinal cord.
To their surprise, only one variant had made it to the brain. The others hadn’t crossed the body’s blood-brain barrier. That’s important, Hughes notes. All of the EEEV copied by the woman’s brain cells would now carry this variant’s genetics.
This seems to suggest that a mix of variants in the blood allows EEEV “to infect different areas of the body,” says Hughes. Her team shared its findings in the July 2021 Emerging Infectious Diseases.
While EEEV cases are rare, rabies infections are not. According to the World Health Organization, rabies kills an estimated 59,000 people each year. Some 95 percent of these deaths occur in Africa and Asia, especially India.
Although dog bites are the leading source of human infections, other animals carry the virus too. Indeed, some variants of rabies virus are well-suited to infect particular hosts. These include racoons, bats, foxes and skunks
Ryan Wallace, who works for the CDC in Atlanta, Ga., studies rabies. He led a 2014 project that looked at how often variants of the virus cross over from rabies-infected animals to other species in the United States.
Scientists had thought rabies variants tended to be linked to one primary species. Such species are known as its “reservoirs.”
In their study, Wallace and his team looked for crossovers into species other than the reservoir. And this proved surprisingly common, they found. For instance, between 1990 and 2011, some 67,058 raccoons were found with the raccoon variant. Another 30,876 other rabid animals also were infected with the raccoon variant.
Crossovers to other species by the raccoon variant “was unexpectedly high,” they reported. Skunks are a major source of rabies. However, compared to skunks, this study found “raccoons were four times more likely to transmit rabies to other species.”
This finding makes a good case for vaccinating pets, Wallace and his coworkers argue. Why? The spillover of a rabies variant from one species to another can lead the virus to adapt into new strains.
These can now more readily attack new host species. The good news: For now, the rabies shots given to dogs and cats work against all U.S. rabies variants.
(Copyright: www.sciencenewsforstudents.org)














Facebook Comments